OzSAGE Residential Aged Care Facility Outbreak Checklist
16/10/2023
OzSAGE Advice Document : Residential Aged Care Facilities: Additional recommendations and tips for managing airborne disease (COVID, INFLUENZA, RSV and other diseases)
Thoughtful and prompt actions taken by Residential Aged Care managers can reduce the impact of COVID-19 and other respiratory diseases in these facilities.
The Commonwealth has provided guidelines to mitigate the impacts of COVID-19 and acute respiratory disease in residential aged care. States and Territories have also published public health advice.
This advice supplements that important government advice by making some additional important points.
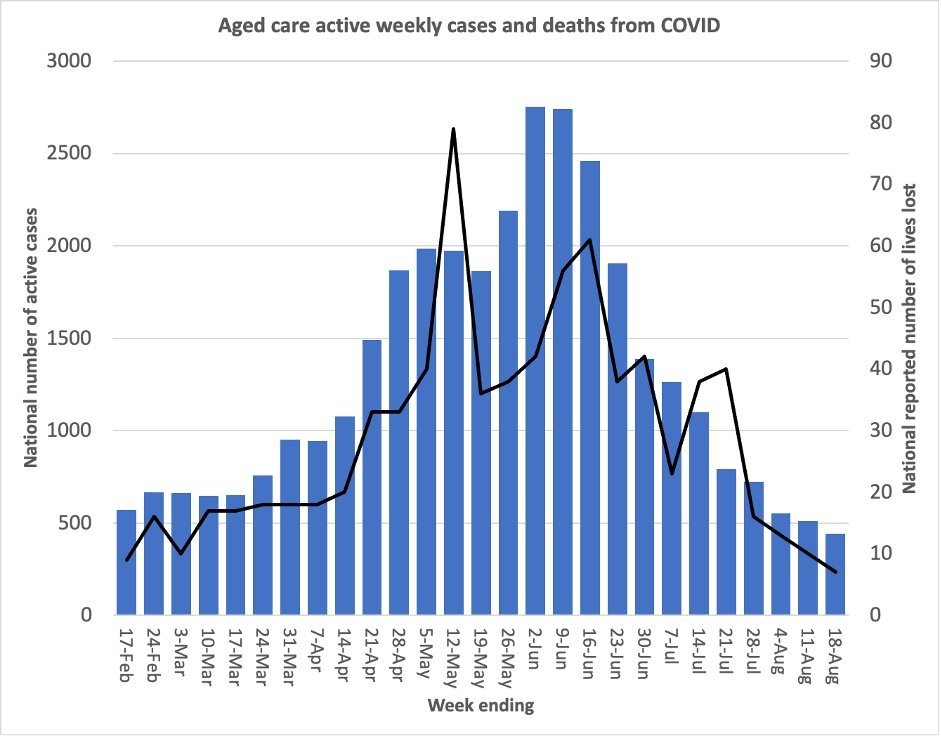
We note protection of residents must remain a priority, as seen from the effect of the recent wave of COVID in residential aged care facilities in the graph below.
Source of raw Data : COVID-19 outbreaks in Australian residential aged care facilities – Australian Commonwealth Government
Improving controls also protects the workforce from absence, and preserves safe and effective running of the residential aged care facility.
OzSAGE provides some additional recommendations on useful actions to prevent and assist the control of outbreaks in residential aged care below:
PRIOR TO OUTBREAKS
Safe indoor air is crucial. OzSAGE has produced evidence-based recommendations for improving indoor air quality. Indoor air should be kept as free as possible from airborne pathogens, including SARS-CoV-2, by improving ventilation and filtration. Portable HEPA air purifiers should be used when CO2 monitoring indicates that CO2 is over 800 parts per million [ppm] in spaces with mechanical HVAC systems. This is not aiming to reduce carbon dioxide itself – this will not happen – but rather to clean air that is demonstrated by persistent high CO2 to be potentially contaminated.
Provide onsite vaccination for residents and staff and ensure all relevant vaccines are up to date (including for COVID-19 and influenza).
Have a plan in place for residents regarding choice of, and access to anti-viral medication ins consultation with the supporting medical staff.
Have available sufficient high-quality air purifiers with HEPA filters to deploy in rooms of infected persons as required.
Mandatory masking of staff and visitors with provision of respirators of quality standard such as P2, N95 or KF94 ( “Analysing different exposures identifies that wearing masks and establishing COVID-19 areas reduce secondary-attack risk in aged-care facilities”, “The effectiveness of non-pharmaceutical interventions on outbreaks of COVID-19 in aged care and long-term care facilities: A meta-analysis”) – except for rare circumstances where medical conditions that prevent mask use. Systematic respirator fit testing for staff is recommended.
Rapid Antigen Testing (RAT) testing policy and provide RATs to staff and visitors to reduce risk of introducing disease into RACF.
Have signage in place and signs available to deal with outbreaks.
Regular pandemic and epidemic outbreak scenario practice exercises and analysis of gaps is recommended.
Systems of staffing changes for outbreaks explained to staff in advance.
Have a clear process for families who wish to take residents out of the facility and back to their homes in an outbreak.
Outbreak should be declared according to Commonwealth and State guidelines (residents and staff). If guidelines are based on testing of residents only, and not staff, maintain a high index of suspicion that there is an outbreak if any staff have positive tests or are unwell.
DURING AN OUTBREAK
When it becomes clear that a resident or staff member is likely to be infected with an airborne disease, in addition to Commonwealth and State advice, consider
First 60 minutes
Designate senior person to be Outbreak Manager to make sure all of the 60 minute list happens
Put up the signage needed for the outbreak control action, including that for relevant resident rooms
Targeted air purifier – HEPA deployment if the source is obvious
Stop all social activities involving congregations
Mandate N95/P2/KF94 respirators and goggles or face shields, for all staff on floor and any essential visitors
Open windows in naturally ventilated rooms and shut resident doors where possible.
Make sure bathroom fans are switched on where device capacity permits continuous operation
Separate ingress and egress between wings if possible
Minimise the number of staff in contact with residents, eg consider care staff instead of kitchen staff delivering food to rooms
Non-critical/non-essential staff such as visiting trades/hairdressing activities to stop, and educate those staff to monitor for symptoms and test
Notify GP regarding anti-viral medication provision
First 6 hours
Shut social areas, and remove seating to avoid congregations. People to eat outside or in own room whenever possible
PPE should be made available at easily accessible stations and doffed in outside air with hazard waste bins
Education of staff re avoiding cross transmission between staff working in outbreak area with those working in areas not affected by outbreak, eg by avoiding car pooling
Post signage for example with instructions for reduced numbers of people in bathroom/change room areas or lifts
For visitors that are vital to well-being, arrange designated outside areas or well ventilated areas with social distance where possible.
First 12 to 24 hours
Arrange lifestyle team to visit rooms in appropriate PPE – prioritising the most vulnerable
Routine checks that meals have been consumed (turn on audit process for “meal not eaten”)
Outbreak Manager (twice a day, morning and after dinner)
Role model and coach good infection control behaviour
Check N95/P2/KF94 respirator appropriate use – educate
Check the layout of seating in spaces
Check “infection control” notice and advice for resident doors is up-to-date
Review “meal not eaten” list and redirect trained staff in PPE to assist
Communicate with any visitors on floor about importance of precautions
Ensure stocks of PPE and RATs remain available
Systematic monitoring of updates and advice of Commonwealth and State Health on their websites
Ensure resident has negative RAT to exit isolation
OzSAGE advises a cautious and prudent approach to declaring that an outbreak is over.
ENDS